
MF2C’s First Patient Sponsor – Zachary Spishock
For seven years, I was living with a mass in the center of my right hand that I believed came about after playing baseball and other sports for many years prior. That all changed on March 30th, 2023, when I finally made the wise decision to call an orthopedic surgeon and get their opinion.
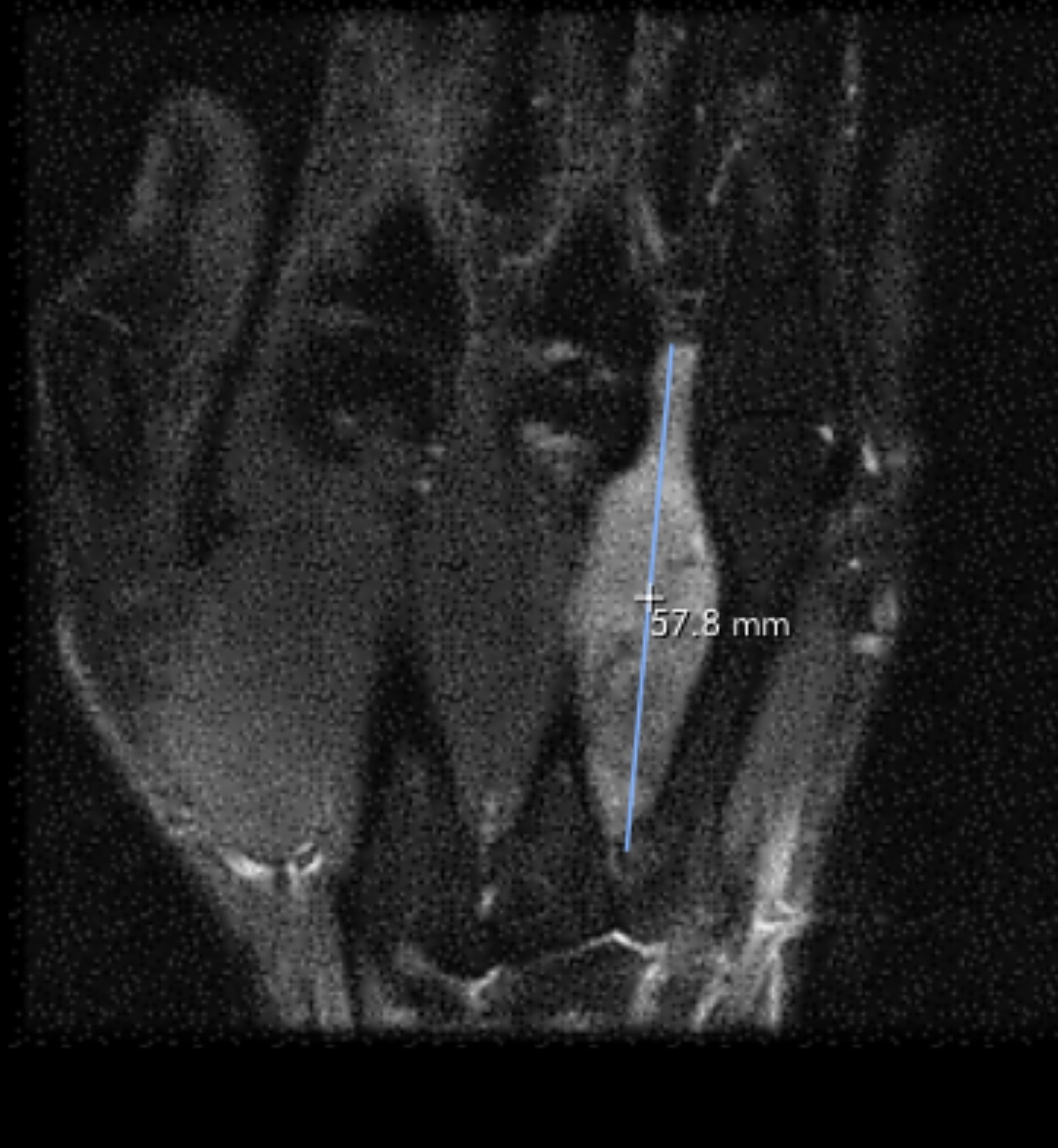
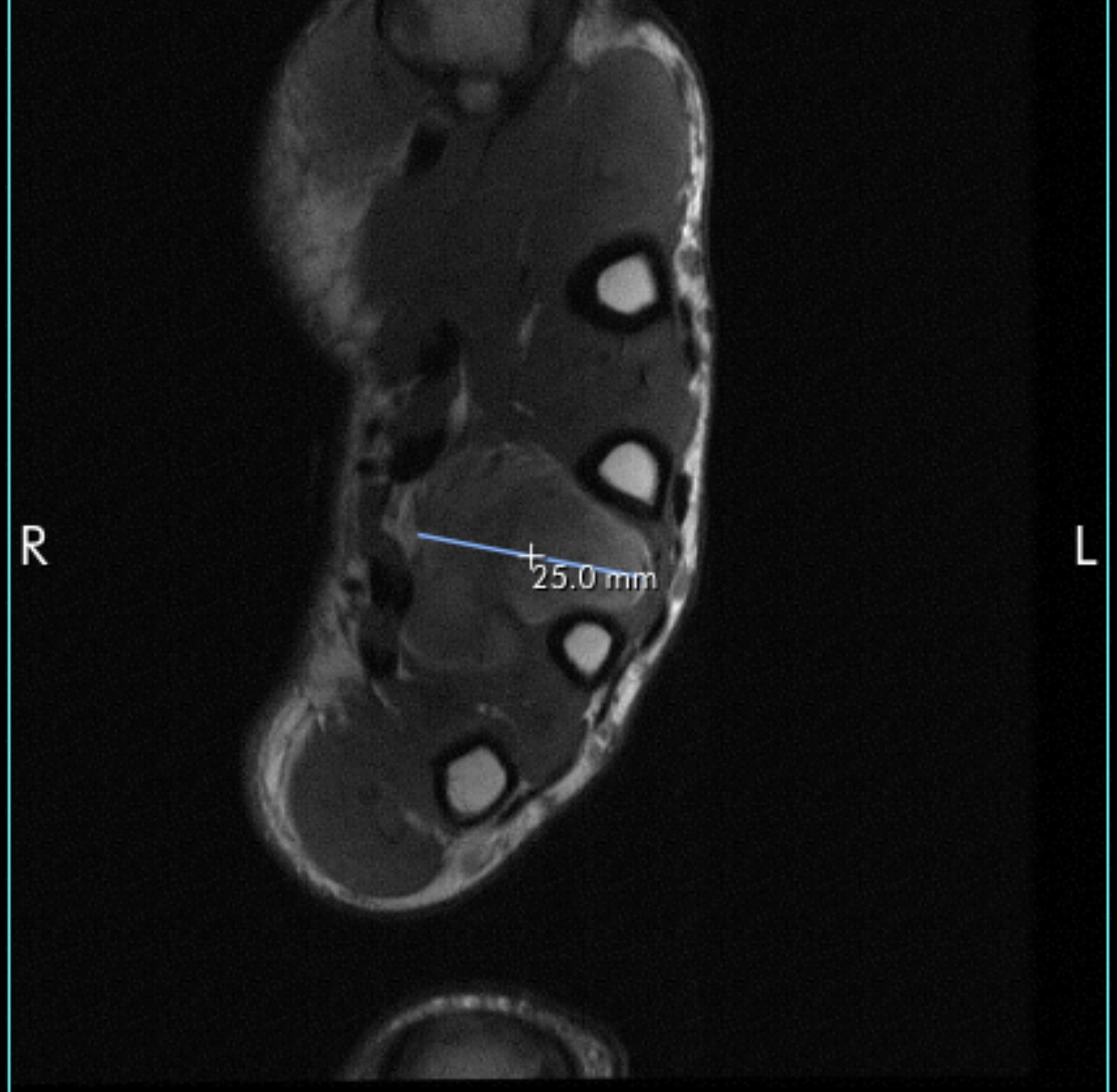
Weeks later, I met with Dr. Ryan Coyle, a board-certified orthopaedic surgeon, who specializes in hands and upper extremities. His findings started concerning me. The mass in my hand lit up significantly. After doing an ultrasound and an x-ray, Dr. Coyle suggested that I get an MRI to further explore the mass. The results were shocking, and I was informed that I needed to get a biopsy from Memorial Sloan Kettering Cancer Center in New York City to confirm the findings. I was sent away with my x-ray and MRI in hand, as well as the names of two doctors to which Dr. Coyle recommended I see.

May 18th, 2023 was the first time I met Dr. Edward Athanasian, a 30-year veteran and specialist in orthopedic hand surgery. We spoke about the best and worst outcomes for my situation, leaving nothing off the table. The possibility of the mass in my hand being malignant was less than 1%, so everyone told me not to worry as I was going to be fine.
A week later my family and I returned to New York City for my follow-up appointment, hoping to hear good news about my biopsy. “It’s malignant,” Dr. A explained. I could feel the emotions coursing through my body, but I stayed strong. With my mother and father both devastated, Dr. A asked, “Are you alright? How are you taking it?” and I told him, “I’m fine, let’s do this.” He could tell right then and there how strong I was going to be through all of this, and he knew he had a fighter in the ring. My diagnosis was Stage 3 Monophasic Synovial Sarcoma – a rare type of cancer that has only been reported in a few hundred people ever in the hand/wrist area.
The next steps were clear, and Dr. A presented a strong case about how to handle the cancer. Radiation and chemotherapy alone wouldn’t be able to shrink the mass enough to avoid having to amputate fingers or worse, my hand. I would need a different procedure, but the catch was that this procedure couldn’t be performed in the United States due to the FDA not approving it along with “Big Pharma,” and I’d be required to get this treatment uninsured. Therefore, I’d have to travel to Prague, Czech Republic to get a treatment called Isolated Limb Perfusion (ILP). I agreed to go forth with his plan.
During one of my appointments, Dr. A’s nurse, Roe, offered to give me the phone number of a man by the name of Trent Twaddle. Little did I know, this man would be the rock throughout my entire journey. After the long train ride back home, I sat in my room puzzled for some time while my parents waited outside. It was then that I decided to make the first phone call to Trent. After an hour or so, I decided to share the details of my conversation with my upset parents. After telling them how much Trent and MF2C were willing to contribute to my case, it brought tears to our eyes. Without MF2C, I would have never been able to travel abroad to receive treatment I needed to not only save my hand, but also my life.

Fast forward to June 20th, 2023 where my mother and I were now in Prague at VFN hospital to meet with Dr. Jan Lesensky, who is the surgical chief for orthopedic oncology (similar to Dr. A in title) and Dr. Miroslav Spacek, my cardiac surgeon responsible for the ILP procedure. After doing blood work and other tests, we discussed the procedure I was going to have. They explained how this procedure actually worked, as well as possible issues that could occur during the procedure – one of which could involve amputation of my limb. We spoke about studies involving my diagnosis, but data was so limited on soft tissue sarcomas that my data would be used to help doctors build a case to help treat future patients with Synovial Sarcoma. I was told that I was the third American to receive ILP in Prague since they began treatment in 2009. The biggest challenge they would face was that I was going to be the first patient ever treated with ILP that included abnormal anatomy, as I had high bifurcation of the brachial artery in my shoulder. Even though this presented challenges with possible blowout and collapsing of my arteries during surgery, Dr. Spacek still committed to do the best he could to treat me either way. 10 days later we boarded a plane to return home from a successful surgery with no complications.

As soon as we landed in the United States, I saw Dr. A in New York so he could examine the surgical treatment and advise of any possible side effects. He explained how his next course of treatment would usually be radiation, but given the size and location of my tumor, we needed to consult an additional oncologist to consider chemotherapy as an option as well. When asked if a Synovial Sarcoma patient had ever received chemotherapy following ILP, Dr. A informed me that I would be the first. After further discussion with Oncologists regarding chemo, they ultimately decided that the chemo wouldn’t be done in efforts to shrink the tumor, but to give me the possibility of a longer and healthier life. Synovial Sarcoma has a proven track record for not responding to any types of chemo. However, there was one option I was offered – AIMs, which is typically referred to as the “red devil chemo” because of its distinctive color and because it can cause serious side effects, including potential heart damage.



The doctors explained all the potential side effects, including blood related cancers from this chemo, as well as long-term life effects that included infertility and possible heart failure. Ultimately, my oncologist and I both agreed that it would be safer to do this now with hopes of preventing the possibility of the cancer spreading, or to kill it if it did spread at all, rather than regretting the choice years later from recurrence. Synovial Sarcoma is known as a “slow growing, fast to spread” cancer, and that is why so many people will go years without noticing the abnormality on their body. Having chemotherapy performed was to give me a longer life If I was able to survive this, and I wasn’t afraid of what came next.

And so it began on July 24th, 2023. The next four months of my life would be utter hell as I received “the devils drug” in an effort to save my life. I received a total of six cycles of AIMs, the lifetime limit of this drug, due to its known potential for causing heart failure issues.
My cycles were as such; treatment for ten hours a day Monday thru Wednesday, followed by hydration for an hour on Thursday and Friday mornings (noted as the worst day of the cycle), with twenty-one days in between cycles (three weeks). This went on for approximately four months, finally concluding my chemo treatments in early November 2023. Some of the side effects I experienced included nausea, vomiting, loss of appetite, hair loss, fatigue, pain, constipation, and much more. The first round I was hospitalized due to trouble breathing and dehydration, with my heart rate reaching 240 beats per minute. We soon realized how important hydration was following chemo, and that made each of the cycles a little easier on me when I would hit my worst days. When the worst was finally behind me, we waited two weeks before we began molding a cast for my hand in preparation for radiation therapy.
That was when I met with Dr. Alektiar, a colleague to Dr. A, and a radiation oncologist known for conducting some of the best research about how to use radiation to shrink tumors before surgery. We were aiming for a home run at this point, as Dr. A knew we needed the tumor to shrink considerably if we had any chance of saving my hand. After mapping out the locations with tattoos and building the mold, I then received twent-five rounds of radiation directly to my hand for five weeks straight. At first, it wasn’t too bad, but then the burns on my skin started to get worse. Thanks to Trent’s suggestion, I started using Biafine Emulsion Cream. A medication that both he and Jake used on their hands to relieve the pain caused by radiation burns.

Jump forward to February 9th, 2024. Sitting with Dr. Athanasian, we reviewed my MRI and determining my surgery procedures. The good news – my tumor had shrunk significantly from radiation therapy, and there was a slight chance that he might be able to save all of my fingers! The bad news – there were four possible surgeries that I would need to receive in order to make saving my fingers a possibility. Iliac bone crest graft, an open reduction tendon graft, an intender fixation nerve graft, and lastly ligament reconstruction were all recommended. Even if we had to do all of these surgeries, Dr. A couldn’t guarantee he could save my hand until he opened me up.
Seven hours later, I opened my eyes and turned my head to look at what was left of my hand. To my surprise, everything was still there and functioning. Dr. A walked in minutes after with the biggest smile on his face and told me that he was able to save everything. In doing so, I lost half of the bone in my ring finger, one-third in my middle finger, as well as a nerve, a ligament, and all the muscle to my ring finger. He installed a metal plate with seven screws to give structure back to my ring finger. He used supplemental nerves and ligaments from my middle finger to supply function to my ring finger, and he took the muscle from my thumb to give strength back to my ring finger. To this day, Dr. A tells me he pushed the limits of what he felt comfortable with when it comes to hand surgeries. But, in all, I know that this decision was made because he knew how hard I fought to keep the hand from the beginning, and we were all in when it came to saving my hand. Three weeks following surgery my biopsy results came back from the tumor sample, and it was found to have negative margins. Dr. A told me that I was in the clear, and I was officially cancer free!




Six weeks post-op, I now had complete feeling in all of my fingers again – something the doctors told me I wasn’t going to get back entirely. The surgical wound had healed incredibly, and thanks to physical therapy (three days a week), I’d regained some strength and functional ability in my hand, which was faster than we thought possible. My original diagnosis in May of 2023 was that I was going to lose one to two fingers, and possibly the complete dexterity and function of my right hand due to the need for a double ray amputation. I believe that the ILP started the process of killing the tumor in my hand, the chemotherapy prevented any of the cancer cells from spreading, killed off cancer cells in my entire of body, and the targeted radiation managed to shrink the tumor enough to consider the possibility of saving my entire hand in surgery.


Thanks to Dr. Athanasian’s surgical touch, we were able to accomplish something unimaginable. But, truth be told, I would have never been able to accomplish any of this if it weren’t for Trent and Middle Finger To Cancer’s support. My decision to call a random stranger, who I knew nothing about, the day I was diagnosed was the uplifting energy and encouragement I needed when I was at the lowest point of my life. Trent guided me through the path that he once walked and gave me the strength and courage to go through this battle, no matter the outcome.
I’m truly blessed to be MF2C’s first sponsored patient. It has meant the world to me. Since the beginning of my battle, I’ve looked forward to helping the next person the same way MF2C has helped me. The ultimate goal is to get ILP approved in the United States, and for the FDA to approve the use of this anticancer drug so that doctors can perform the same, or similar, lifesaving surgeries without having to other countries. The obstacles that Trent and I had to overcome could all be eliminated if this treatment were available in the United States – making it easier for patients to afford the treatment, but more importantly, give them the option to save their limbs.
The simple fact that this treatment saved my hand when it wasn’t even a possibility speaks volumes. 185,000 people lose their limb every year in the United States. 3,700 of those are due to cancer. That’s 10 people per day who never had the opportunity to save their limb due to the lack of treatment options available in the United States. How would you feel if this were you or someone you loved? I didn’t have to give my middle finger to cancer, so I give two middle fingers to cancer!
Help us by joining the fight and give the Middle Finger to Cancer!


Recent Comments